Introduction:
Cancer remains one of the most challenging diseases to treat, with conventional therapies often falling short in controlling its progression. However, CAR-T therapy emerges as a game-changer in cancer treatment, offering a novel approach that harnesses the power of the immune system. In this comprehensive guide, we'll delve into the fundamentals of CAR-T therapy, its mechanisms of action, benefits, potential risks, eligibility criteria, associated costs, and the promising future it holds in the fight against cancer.
What is CAR-T Therapy?
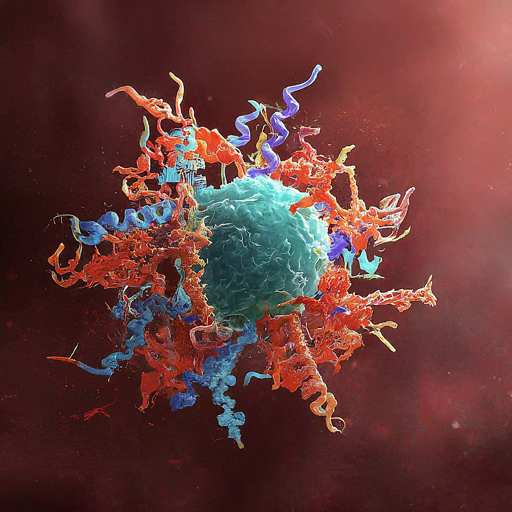
CAR-T therapy, or chimeric antigen receptor T-cell therapy, represents a groundbreaking immunotherapy approach that utilizes genetically modified immune cells to target and eliminate cancer cells. These modified T cells are engineered to express chimeric antigen receptors (CARs), which enable them to recognize and attack specific proteins present on the surface of cancer cells. CAR-T therapy primarily targets blood cancers such as leukemia and lymphoma, where traditional treatments may have limited efficacy.
History and Development of CAR-T Therapy
CAR-T therapy has its roots in decades of research in the field of immunology and cancer biology. The concept of using T-cells as a therapeutic tool gained traction in the early 2000s, with researchers exploring ways to enhance their ability to target cancer cells selectively. Over the years, advancements in genetic engineering techniques and understanding of tumor biology have paved the way for the development of CAR-T therapy as a viable cancer treatment option.
Types of Cancer Treated with CAR-T Therapy
CAR-T therapy has demonstrated efficacy in treating various types of cancer, including:
- Acute lymphoblastic leukemia (ALL)
- Diffuse large B-cell lymphoma (DLBCL)
- Multiple myeloma
- Chronic lymphocytic leukemia (CLL)
- Pediatric neuroblastoma
Success Stories and Clinical Trials
Numerous clinical trials and real-world applications have showcased the potential of CAR-T therapy in achieving durable remissions and even complete eradication of cancer in some patients. Notable success stories include cases where patients with advanced leukemia or lymphoma achieved long-term remission following CAR-T therapy, despite failing multiple rounds of conventional treatment.
Cancer's Nemesis: The Power of CAR-T Cells
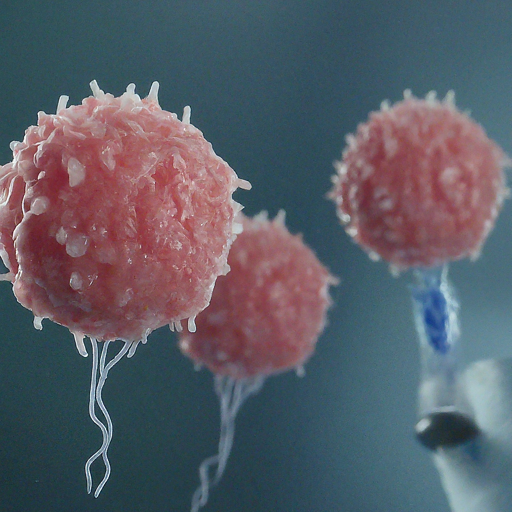
CAR-T therapy operates on a simple yet profound principle: reprogramming the body's own immune cells to seek and destroy cancer. By equipping T cells with specialized receptors, scientists empower them to identify and attack cancerous cells with precision.
How Does CAR-T Therapy Work? CAR-T therapy involves a series of intricate steps:
- Extraction of T cells: T cells are harvested from the patient's blood through a process called leukapheresis.
- Genetic modification: In the laboratory, these T cells are genetically engineered to express CARs, enabling them to recognize cancer cells.
- Cell expansion: The modified CAR-T cells are cultured and expanded to large numbers to ensure an adequate therapeutic dose.
- Reinfusion: The expanded CAR-T cells are reintroduced into the patient's bloodstream, where they can target and destroy cancer cells.
Visual aids such as diagrams or infographics can help simplify the understanding of this complex process.
Empowering the Immune Army: The Journey of CAR-T Cells
CAR-T therapy orchestrates a symphony of cellular interactions, culminating in a targeted assault on cancer. From extraction to reinfusion, each step plays a crucial role in unleashing the full potential of the immune system against malignant cells.
Benefits of CAR-T Therapy: CAR-T therapy offers several distinct advantages over traditional cancer treatments:
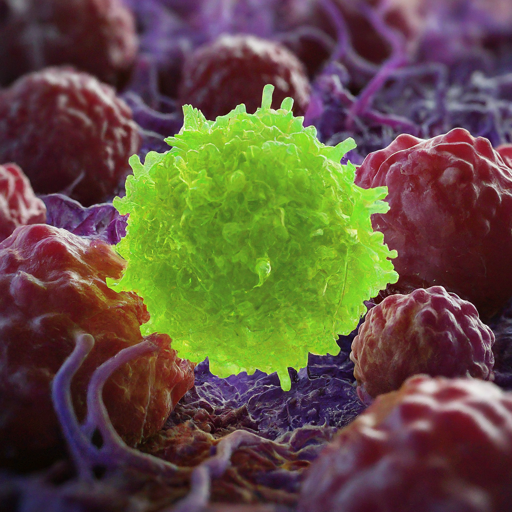
- High specificity: CAR-T cells selectively target cancer cells while sparing healthy tissues, minimizing collateral damage.
- Long-lasting response: CAR-T cells can persist in the body, providing durable immune surveillance and potentially preventing cancer recurrence.
- Personalized approach: CAR-T therapy utilizes the patient's own immune cells, reducing the risk of rejection and allowing for personalized treatment strategies.
While these benefits are promising, it's essential to acknowledge potential risks and limitations associated with CAR-T therapy.
Side Effects and Risks: Like any medical intervention, CAR-T therapy carries inherent risks and potential side effects. These may include cytokine release syndrome (CRS), neurotoxicity, and increased susceptibility to infections. However, healthcare providers employ various strategies to monitor and manage these risks, ensuring patient safety throughout the treatment process.
Navigating the Terrain: Understanding CAR-T Therapy's Side Effects
As with any revolutionary treatment, CAR-T therapy comes with its share of challenges. From cytokine storms to neurological complications, healthcare teams remain vigilant in mitigating risks and optimizing patient outcomes.
Who is Eligible for CAR-T Therapy? Eligibility for CAR-T therapy depends on several factors, including the type and stage of cancer, previous treatments, and overall patient health. Ongoing research aims to expand eligibility criteria and improve accessibility to CAR-T therapy for a broader range of patients.
CAR-T Therapy Costs: One significant challenge associated with CAR-T therapy is its high cost, which may pose barriers to access for some patients. Efforts are underway to address affordability issues and advocate for improved insurance coverage to ensure equitable access to this life-saving treatment.
The Future of CAR-T Therapy: The landscape of CAR-T therapy continues to evolve rapidly, with ongoing research efforts focused on:
- Expanding Indications: Exploring CAR-T therapy's efficacy in additional cancer types beyond hematologic malignancies.
- Enhancing Safety and Efficacy: Refining the therapeutic approach to mitigate side effects and optimize treatment outcomes.
- Improving Accessibility: Innovating strategies to reduce costs and enhance accessibility to CAR-T therapy for a broader patient population.
Conclusion:
In conclusion, CAR-T therapy represents a transformative advancement in cancer treatment, offering a personalized and targeted approach with the potential for durable responses. By harnessing the power of the immune system, CAR-T therapy has revolutionized the way we combat certain types of cancer, providing new hope for patients who have exhausted conventional treatment options. While challenges such as high costs and potential side effects remain, ongoing research and collaborative efforts are driving progress towards broader accessibility and improved patient outcomes.
It's crucial for individuals affected by cancer to stay informed and explore all available treatment options, including CAR-T therapy, in consultation with their healthcare providers. As the field of CAR-T therapy continues to evolve, with advancements in technology and scientific understanding, we can look forward to a future where this groundbreaking treatment becomes more accessible and effective for patients worldwide.
CAR-T Therapy: A Beacon of Hope in the Cancer Landscape
Unleashing the Potential of CAR-T Therapy: Revolutionizing Cancer Treatment
In the realm of oncology, CAR-T (Chimeric Antigen Receptor T-cell) therapy stands as a beacon of hope, heralding a new era in the fight against cancer. This innovative approach represents a paradigm shift, harnessing the body's own immune system to target and eradicate cancer cells with unprecedented precision and efficacy. As research continues to unravel the complexities of cancer biology and immunology, CAR-T therapy emerges as a transformative force, offering new hope to patients facing daunting diagnoses.
Understanding CAR-T Therapy: A Triumph of Precision Medicine
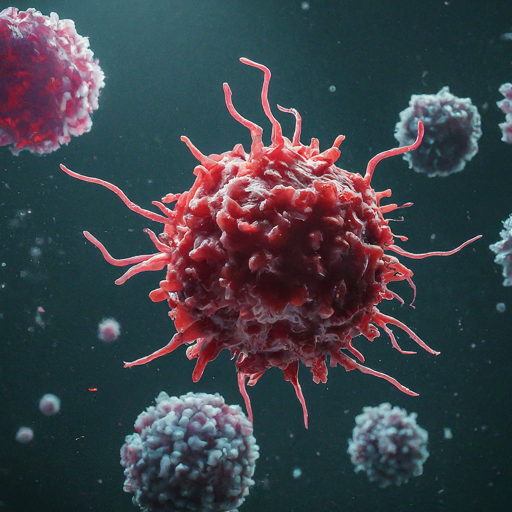
At the heart of CAR-T therapy lies a remarkable feat of genetic engineering and immunology. The process begins with the extraction of a patient's own T-cells, a type of white blood cell central to the immune response, from their bloodstream. These T-cells are then genetically modified in the laboratory to express chimeric antigen receptors (CARs) on their surface. These CARs are designed to recognize specific proteins, or antigens, that are commonly found on the surface of cancer cells.
Once engineered, the CAR-T cells are multiplied to generate a robust population capable of mounting a potent immune response. The expanded CAR-T cell population is then infused back into the patient's bloodstream, where they navigate the body in search of cancer cells bearing the targeted antigen. Upon encountering cancer cells, the CAR-T cells become activated, initiating a cascade of immune-mediated destruction that specifically targets and eliminates cancerous cells while sparing healthy tissues.
Clinical Success and Applications: Pioneering Triumphs
The clinical success of CAR-T therapy has been nothing short of remarkable, particularly in the realm of hematologic malignancies. In particular, CAR-T therapy has demonstrated unprecedented efficacy in the treatment of certain types of leukemia and lymphoma, leading to significant rates of complete remission and durable responses in a subset of patients.
Notably, CAR-T therapies such as Kymriah® (tisagenlecleucel) and Yescarta® (axicabtagene ciloleucel) have received regulatory approval for the treatment of relapsed or refractory B-cell acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL), respectively. These milestones underscore the transformative potential of CAR-T therapy in reshaping the treatment landscape for patients with limited therapeutic options.
Expanding Horizons: Challenges and Opportunities
Despite its remarkable successes, CAR-T therapy is not without challenges. One significant hurdle lies in the management of adverse events, including cytokine release syndrome (CRS) and neurotoxicity, which can occur as a result of the robust immune response triggered by CAR-T cells. Efforts to optimize the safety profile of CAR-T therapy through improved patient selection, prophylactic interventions, and enhanced monitoring protocols are ongoing.
Moreover, the high cost and logistical complexities associated with CAR-T therapy pose barriers to widespread adoption and accessibility. From the intricate manufacturing processes to the specialized infrastructure required for administration and patient monitoring, CAR-T therapy presents unique challenges that necessitate collaborative efforts across academia, industry, and healthcare systems to overcome.
Nevertheless, the potential of CAR-T therapy extends beyond hematologic malignancies, with ongoing research efforts exploring its applicability in solid tumors. While solid tumors present distinct challenges, including the immunosuppressive tumor microenvironment and heterogeneous antigen expression, innovative strategies such as combination therapies, engineered CAR designs, and targeted delivery mechanisms offer promising avenues for overcoming these obstacles.
Charting the Course Forward: Collaboration and Innovation
The advancement of CAR-T therapy hinges on interdisciplinary collaboration, scientific innovation, and a steadfast commitment to patient-centric research. From refining manufacturing processes and optimizing treatment protocols to exploring novel targets and therapeutic modalities, the journey towards unlocking the full potential of CAR-T therapy is multifaceted and dynamic.
Moreover, regulatory agencies play a pivotal role in ensuring the safety, efficacy, and accessibility of CAR-T therapies through rigorous oversight and expedited review processes. By fostering a conducive regulatory environment that encourages innovation while safeguarding patient interests, regulatory bodies contribute to the translation of scientific discoveries into transformative therapies that benefit patients worldwide.
Looking to the Future: A Vision of Hope
As we stand on the precipice of a new frontier in cancer treatment, the promise of CAR-T therapy shines brightly, illuminating the path towards a future where cancer is no longer synonymous with despair but with resilience, innovation, and hope. With each breakthrough and milestone, we inch closer to realizing a world where every patient has access to personalized, precision therapies that offer not only a chance at survival but a quality of life unencumbered by the burden of cancer.

In conclusion, CAR-T therapy stands as a testament to the power of human ingenuity, scientific discovery, and collective determination in the face of adversity. As we continue to unravel the mysteries of cancer and harness the innate capabilities of the immune system, CAR-T therapy represents a beacon of hope for patients, families, and healthcare providers alike, inspiring us to push the boundaries of what is possible and redefine the future of cancer care.
FAQs (Frequently Asked Questions)
What types of cancer can be treated with CAR-T therapy?
CAR-T therapy is primarily used to treat certain types of blood cancers, including B-cell acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL). Research is ongoing to explore its efficacy in other cancer types, such as solid tumors.
How effective is CAR-T therapy in treating cancer?
CAR-T therapy has shown promising results in clinical trials, with some patients achieving complete remission or long-term disease control. However, its effectiveness can vary depending on factors such as the type and stage of cancer, as well as individual patient characteristics.
What are the potential side effects of CAR-T therapy?
Common side effects of CAR-T therapy include cytokine release syndrome (CRS), neurotoxicity, and prolonged cytopenias. These side effects can range from mild to severe and may require medical intervention. Healthcare providers closely monitor patients during and after treatment to manage any adverse reactions.
Is CAR-T therapy covered by insurance?
Insurance coverage for CAR-T therapy varies depending on factors such as the patient's insurance plan, the specific CAR-T product used, and the indication for treatment. Patients are encouraged to work with their healthcare providers and insurance companies to understand their coverage options and potential out-of-pocket costs.
What is the cost of CAR-T therapy?
The cost of CAR-T therapy can be substantial, with treatment expenses including the cost of the CAR-T product itself, hospitalization, supportive care, and monitoring. While efforts are underway to address affordability issues and improve insurance coverage, the high cost of CAR-T therapy remains a significant barrier for some patients.
Are there any long-term effects of CAR-T therapy?
Long-term effects of CAR-T therapy are still being studied, as the treatment is relatively new. Some patients may experience prolonged remission or even cure, while others may require additional treatment or experience disease recurrence. Continued monitoring and research are essential to understand the long-term outcomes of CAR-T therapy.